
Taking regular medicines is common, and it’s not unusual for people to miss an occasional dose or take it outside the regular time window. Forgetting to do something is normal, but in the case of medicines, forgetting to take them at the prescribed time can have negative health effects.
By one estimate, about half the population of people taking regular medicines don’t take them as prescribed. Is this a breakdown in communication? A lack of understanding of their importance? Forgetfulness?
Largely, reasons for not taking medicines as prescribed can be organised into two types: intentional and unintentional.
Unintentional is when a patient intends to follow the prescribed regimen but doesn’t due to factors outside their control, including forgetfulness, difficulties understanding dosing instructions, or cost.
But for some, a patient consciously decides not to follow the prescribed regimen. This could be due to side effects, or not believing in the necessity of the medicine.
Medication-taking is complex because each person is unique and the challenges to each person’s medication-taking can vary quite significantly. The most effective strategy is one that also considers why a person isn’t taking their medicine. What are some of the support strategies available, and are they actually helpful?
Pill boxes
The most commonly used methods to support medication adherance are organisational strategies such as days-of-the-week pill containers.

These are functional if a patient has to take many different medications.
But they’re not always suitable – if the user does not fill the container correctly or doesn’t remember to collect the prefilled pack (called a Webster-pak, blister pack or dosette box) from the pharmacy, this simple intervention quickly becomes ineffective.

Some medicines can’t be packed because their stability is compromised with repacking, and patients with reduced eyesight or dexterity can struggle to use these containers.
So while they are an effective prompt, simple reminder cues such as days-of-the-week pill containers may not be ideal for everyone.
Alarms
Pre-set alarms are another commonly used reminder method.
However, this strategy is not infallible, and the literature shows many patients miss medication doses when out of routine because they turn their alarm off subconsciously when occupied with another task.
Reminder alarms only seem to be effective when they are interactive or personalised.
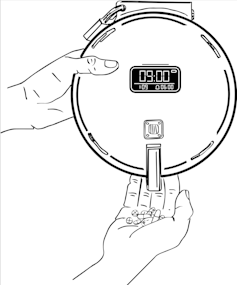
For example, in a handy combination of both methods above, you can now buy automated pill dispensers with alarms that go off at predetermined times and only stop when the medication is removed.
These can be especially handy for those with memory issues such as dementia. However, they are not cheap, costing a few hundred dollars each, and so will not be accessible for everyone.
Mobile apps
The latest Apple iOS update allows you to track your medications and schedule reminders.
Medication reminder apps were first developed to support older adults and people with chronic diseases required to manage multiple medicines.
But they’ve now been embraced as a suitable support for anyone wishing to independently manage their own medicines, including those on short-term medicines such as antibiotics.

They provide simple, practical health-specific information as well as supporting medication-taking through automation.
According to The Royal Australian College of General Practitioners, a lot of patients like receiving reminder prompts through an app, and it helps them remember to take their medication.
Although the platforms differ slightly, the general premise is a patient independently inputs their medication-taking and prescription refill schedule, and the app then generates automatic reminders for the patient.
The only downside is like any notification, they can be easily dismissed or overlooked.
Habit stacking
When our day changes, for example if we go out for brunch and we usually take our medicines with breakfast, or an unexpected visitor arrives at the usual 11am pre-lunch tablet time, often we forget our medications. This is where “habit stacking” may be beneficial.
Although habit stacking is a relatively new approach to fostering medication taking, habit formation has been repeatedly shown to effectively support wellbeing. Linking medication-taking to a behaviour that does not change from day to day, such as cleaning your teeth, or removing shoes when entering the house, can help you to remember medications.
Some more habit stacking examples to support medication taking may include:
• hygiene routine – shower, shave, swallow
• after dinner unwind – cuppa and meds
• morning mantra as you leave the house – keys, phone, wallet, meds.
What else can we do?
We are all unique, so to make sure we actually take our medicines we need to find what works for us, and consider why we weren’t actually taking them in the first place.
Reminders, gadgets, habit stacking, or a combination may help. We need strategies that can adapt to the unexpected.
Amelia Cossart does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
* This article was originally published at The Conversation

0 Comments