
Sixteen-year-old Karl is seen for the first time in my optometry practice. He was referred to me for a fluctuating vision problem. During his examination, I saw signs suggesting he may have diabetes, which could have explained the fluctuating vision. This suspicion became a reality when his family doctor confirmed the diagnosis. Karl’s world was turned upside down.
As an optometrist, I invite you to dive into a reality that should concern us all.
What is diabetes?
Diabetes is an insidious disease. Its symptoms (thirst, need to urinate often, fatigue, weight loss, darker skin areas on the neck and underarms) often go unnoticed, at least in the early stages of the disease.
Diabetes affects the lives of one in 14 people in Canada (7 per cent) and one in 10 in North America (10 per cent).
Two types of diabetes can be diagnosed:
Type 1, which is insulin-dependent and develops when the body cannot produce the insulin needed to metabolize the sugars we ingest and which feed our tissues
Type 2, which develops when insulin is produced, but in insufficient quantities. Sometimes the insulin that is produced is ineffective in doing its job.
Type 1 diabetes is usually associated with the development of the disease in childhood and adolescence. Type 2, the most common, usually develops later in life, often after age 50.
A counter-intuitive diagnosis, but not a rare one
From this definition, it would have been logical to conclude that Karl was affected by Type 1 diabetes, the course and treatment of which are well controlled by physicians. However, in his case, and after the required testing, his doctor identified Type 2 diabetes. This diagnosis is counter-intuitive and poses significant challenges. The speed of onset, the initial severity of the disease and the mechanisms of resistance, or of reduced insulin secretion, may be different in patients who develop the disease at a younger age than in adults.
In addition, treatment options, involving trial and error, become more complex due to the much longer duration of this type of disease when it starts at a young age. Both major and minor changes that affect the blood vessels in the Type 2 diabetic patient can have serious consequences that are difficult to predict since the course of treatment can continue for 40 to 60 years.
However, Karl’s situation is not exceptional. More and more young people and adolescents, especially those who are overweight, obese, and sedentary, are affected by Type 2. Almost 75 per cent of them have parents or siblings with diabetes.
While at first sight, this confirms genetics as a risk factor for developing the disease, in this specific case, it was more a consequence of poor lifestyle habits, especially dietary habits, and lack of physical activity, which are often shared by the whole family.
Impact on vision
The fact that Karl developed Type 2 diabetes earlier, rather than later in life also puts him at a higher risk of developing eye complications. An article about this topic recently caught my attention. This study looked at the records of 1,362 people with diabetes living in Minnesota, so, in North America and then extrapolate to Canada. The data was compiled between 1970 and 2019, which also allows us to measure the evolution of the situation over the last decades.
The results are astonishing: young people with Type 2 diabetes (compared to Type 1 diabetics of the same age) are 88 times more likely to develop retinopathy (abnormal blood vessels and/or hemorrhages in the retina). In addition, the risk of this retinopathy becoming “proliferative,” and therefore threatening to vision, is increased 230 times. There is also a 49-fold increase in the risk of fluid accumulation in the retina (macular edema) and a 243-fold increase in the risk of developing a mature cataract at a young age. The latter requires surgery which is riskier in young people than in the case of age-related senile cataracts.
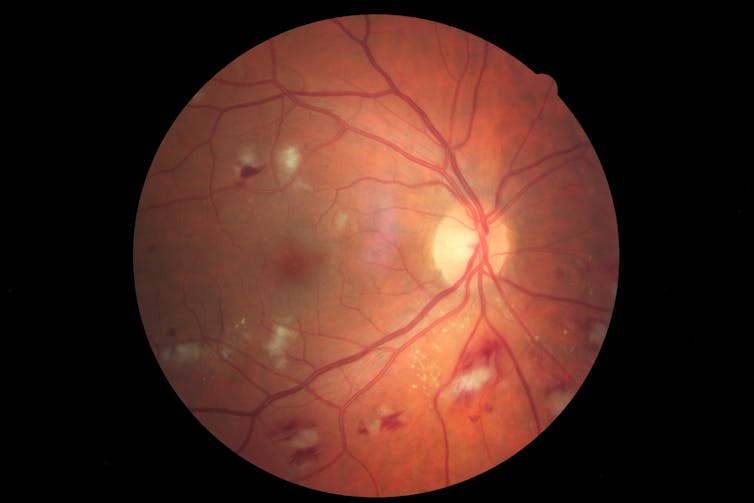
What should we remember from this? That the major problems, which often require surgical interventions to save vision, occur much more rapidly in young Type 2 diabetics than in those affected by Type 1. These patients must therefore be followed more closely. Indeed, almost one in two Type 2 patients will develop some form of retinopathy within one to eight years of diagnosis. In comparison, one in three Type 1 diabetics will develop retinopathy between six and 10 years following diagnosis.
Significant repercussions
Already having increased significantly in the last 10 years, the prevalence (number of cases) of Type 2 diabetes in young people is predicted to quadruple by 2050. This prediction is most alarming for health professionals, but also for policymakers and managers of public health agencies. The lifetime cost of direct medical care for a single diabetic patient aged 25-44 years was US$125,000 in 2013. These costs have since increased and many more dollars need to be added to cover the period between 15 and 25 years, which is not taken into account. Indeed, if 20 per cent of the youth population develops diabetes by 2050, millions (perhaps billions?) of health-care dollars will have to be spent on their care by our governments.
The long-term quality of life of people with diabetes is also reduced. Another study, this time of young people with Type 1 diabetes, shows that their disease has a negative impact on their life. They have to devote a lot of time to their care (missing activities with their friends). And the burden of their disease on their relatives weighs heavily on their shoulders. The fear of hypoglycemia (lack of sugar that can lead to coma) or of developing serious complications of the disease also affects them. Achieving autonomy is more difficult for these adolescents, and their quality of life is proportional to the freedom they can or cannot exercise.
Eat well, exercise and visit your optometrist
Type 1 diabetes is difficult to prevent, mainly because we don’t know all the reasons why it occurs and to proactively screen for it. The situation is different for Type 2 diabetes, which is strongly associated with unhealthy lifestyle in young people. Eating a healthy diet, exercising regularly, and combating sedentary lifestyles, including limiting screen leisure time (to less than two hours per day), are good ways to avoid or delay the onset of diabetes in young people. Screen time is also associated with insulin resistance and obesity in young people. In other words, healthy lifestyles must be encouraged and especially shared within the family unit.

As far as eyes are concerned, regular visits to the optometrist or ophthalmologist can detect early signs of diabetic complications (signs are seen in up to 30 per cent of patients shortly after diagnosis). These health professionals can also detect other oculo-visual problems arising from the disease, such as loss of ability to focus up close (accommodation), partial paralysis of certain muscles of the eye resulting in double vision, delayed healing of surface corneal changes, dry eye or glaucoma. Testing should be done at the time of medical diagnosis of diabetes, or in anyone with a high-risk profile (heredity, obesity, sedentary lifestyle).
Since healthy lifestyle habits are an integral part of the treatment of the disease, it is not too late for Karl to enjoy a happier future. But it is important not to neglect regular follow-ups by his medical doctor and frequent visits to his family optometrist.
Langis Michaud does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
* This article was originally published at The Conversation

0 Comments